Axle Health is a healthcare technology company on a mission to revolutionize home-based care delivery through its comprehensive operations platform. Founded in 2020 by healthcare and technology veterans, including several former Uber executives who brought their logistics expertise to the healthcare industry, Axle Health’s AI-powered logistics platform enables healthcare organizations to efficiently deploy clinicians for in-home visits, improving patient outcomes while reducing operational costs. The company is headquartered in Los Angeles, California.
Sector: Healthtech + Services
Beads
Beads specializes in offering a residential facility for end-of-life care for people who suffer from terminal cancer or intractable neurological diseases, enabling patients to spend their time in a comfortable way.
OncoveryCare
OncoveryCare delivers comprehensive, whole-person care to cancer survivors. As the population of survivors grows rapidly alongside advances in medicine, OncoveryCare provides the personalized, longitudinal care that cancer survivors need to lead happier, healthier lives. Founded by a breast cancer survivor and led by both clinicians and survivors, OncoveryCare’s first offering is a novel Cancer Transitions of Care program, equipping each survivor with a survivorship-trained clinical team and the essential tools and skills they need to actively manage their survivorship journey.
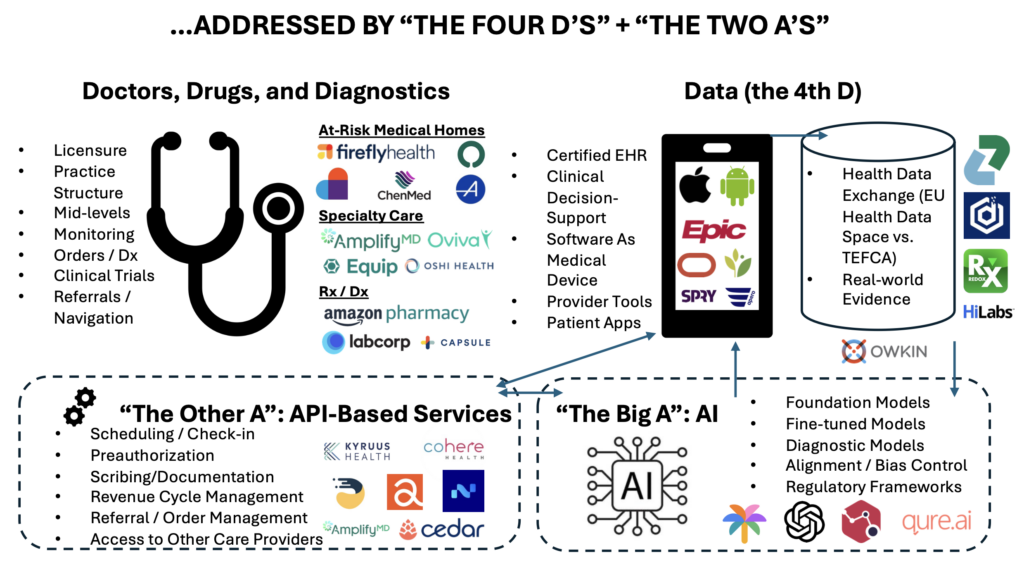
New Digital Care Architecture: The “Four Ds of Digital Health” Meet the “Two As of Automation”
Building on the “Four Ds of Digital Health”, two key automation advancements are being incorporated to make an impact: artificial intelligence and API-based services.
A new digital care architecture is transforming healthcare by integrating the Three Ds of healthcare delivery (doctors, drugs, and diagnostics) with data, AI, and API-based services, creating a more accessible, personalized, and efficient system for both patients and providers.
The modern healthcare delivery system requires a new architecture, powered by technology and tech-enabled services.
Key Trends Demand Systemic Change
Myriad trends are rendering our traditional care delivery system ill-suited to today’s challenges:
– Provider supply constraints cannot meet rising demand
– A system built around acute care is not well suited to managing chronic conditions
– Digital interfaces give rise to new modes of engaging in patient care
– Financing is shifting from fee-for-service to value-based models
– Expensive breakthrough therapies proliferate in pharma, biotech, and medical devices
– Administrative burdens have grown exponentially requiring better infrastructure
The design requirement for a new digital care architecture is clear: care must be more accessible, always-on via multiple channels that mix digital and physical delivery, tailored to the specific care plan of each patient. This requirement cannot be met in a world where traditional delivery systems focus more on consolidation for negotiating leverage than on making care affordable and/or easy to access.
Data as a Key Component of Care Delivery
Data deserves a full seat at the table alongside the traditional Three Ds of healthcare delivery: doctors, drugs, and diagnostics. Indeed, there now are Four Ds of Digital Health. Without accurate, robust, and real time data, it is not possible to get the care you deserve. When care can be personalized, the quality of the data is as important to patient health as everything else.
So, the era of asking “where does it hurt?” and starting from there no longer works because without rich information about your medical history, diagnostic testing, and the full complement of medical records that have accompanied your lifetime of care, practitioners cannot give you the best that medicine has to offer in a way that is convenient, reliable, and efficient. In many cases, your genetic profile, your family history, or insights from prior episodes of care are vital to ensuring that you get the right procedure, the right drug, and/or the right care recommendation.
This goes beyond the testing and data requirements of a given specialist. Yes, GI docs need to know inflammatory marker levels before creating a care plan, and cardiologists need real-time data on cardiac function and fluid status to fine-tune heart failure therapy. But, these providers also need to know what is going on for a patient across the care continuum, including plans and histories of the patient related to conditions other than the specific one they are treating. Similarly, primary care physicians need to know what is happening for a patient in all of these areas, particularly when there are multiple chronic conditions at play. Powered by AI tools noted below, physicians now access patient data via concise, cogent summaries of care episodes without wading through the “PDF graveyard” inside their EHRs (if they have that information available to them at all).
The “Department Store” Model Doesn’t Work
Health systems have responded to data challenges by suggesting simply that all the information should be housed in one medical record in a healthcare environment completely controlled by that one entity. Think of this as the “department store model.” Macy’s had one of everything, so you didn’t need to go anywhere else. Yet, consumers wanted more. They wanted a wider variety of brands, lower price points, and diverse channels. Hence, Amazon came along and former department stores are now being converted into housing for the elderly.
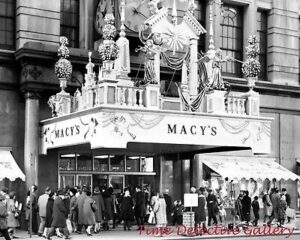
It’s a similar dynamic with health delivery. Large health systems seem to say, “Just never leave my four walls, and everything will be ok.” They hoard data if not required by the government to share it and their technology partners embrace this model. And this works for them. With everything under one roof, they can charge more for everything. Yet, research shows that as health systems get larger, the cost of any one service goes UP not down, while quality deteriorates. Adding insult to injury, patients cannot access these systems readily, due to a combination of supply constraints and process inefficiency. The bill for this inefficient model is borne by society broadly, via higher prices paid by employers, patients, and whoever prints T-Bills in the U.S. Treasury. Remarkably, even when everyone is using the same medical record, outcomes are not better with respect to cost or quality. Even with all the data in one place, the “department store” is still under-gunned compared to the power of the marketplace to deliver cost and quality to the end user (the patient).
A Better Solution: Unbundling Care Delivery, Powered by The Four Ds and Two As
Care delivery needs to evolve so that each patient is seen by the right provider at the right time, in a way that is convenient for patients.
Today, care is bundled in the form of large health systems, in part because the data is disparate and unbundled [1]. Once the data is put in one place and is comprehensive, accessible to anyone at any time, care delivery can be unbundled in a way that enhances value. When companies like Zus Health make data ubiquitous (mediated by privacy and consent) we can step away from data hoarding, mediated by health systems and their legacy technology vendors.
This allows an actual market to develop, so that healthcare can finally benefit from the economies of scale and the power of technology in ways that bear fruit in most other industries. The power of markets to generate new value propositions, breathtaking levels of cost reduction, and delightful consumer experiences is well known. Just look at anything you do with Amazon or e-commerce, buoyed by fintech and advanced logistics, we live in a world where almost anything feels possible in the retail environment.
Health care certainly is different than that. Most patients do not have the knowledge to make accurate shopping decisions in the healthcare context, but that’s changing given the proliferation of AI tools which depend crucially on access to data. Additionally, when data is unified, care can be unbundled, which means that you can seek advice from any care provider, liberating you from the slog of what primary care has become in large health systems today, allowing you to access new modes of care that are better tuned to the realities of life today.
What kills patients is not so much acute episodes or infections, important as those care moments can be, as chronic diseases, best addressed by persistent, more available solutions.
This looks like comprehensive primary care that is more convenient for you because it sits in the palm of your hand, available all the time, provided by companies like Firefly, Oak Street, or Aledade. These “medical homes” take risk for total costs, so they invest in a longitudinal relationship; as “health fiduciaries,” they are accountable both for health and cost. These entities manage their patients proactively, developing rich user experiences for accessing care virtually or in-person and navigating the system on behalf of their patients, including partnerships with specialized care providers. If a patient has an eating disorder, the medical home can ask Equip to address it; GI issues can be handled by Oshi; while patients on a fertility journey access Carrot. This type of dynamic and integrated care provision is made possible when all participants can read from, and write to, the same dataset and coordinate seamlessly. Unlike an all-in-one department store like the Mayo Clinic, this model provides an open network, where a marketplace can emerge with richer, more tailored and higher value services, mediated by an organization accountable for your health and your budget. Fluid data enables this.
The four Ds of digital health will unlock new opportunities for quality and cost improvement and many of the startups featured at the HLTH conference illustrate this. The Four Ds themselves, however, are not enough. That is why I am adding to the framework The Two As of Automation.
The Two As of Automation: “The Big A” and “The Other A”
Automation is about making sure that work is performed reliably, consistently, and in a cost effective way. With automation, care providers and the companies they work with can get things done at the touch of a button, or – better yet – without pushing a button at all.
So, what are the Two As of automation? These can be broken down into “The Big A,” the one everyone can’t stop talking about, which is artificial intelligence. But true transformation of the care delivery system also requires “The Other A,” API-based services. Pranay Kapadia, CEO of Notable, previewed this post and explained that “agents” perhaps could be their own “A” in this framework; they straddle the line between APIs and AI and represent a key innovation vector.
When data is unified and care can be unbundled, then every care provider can operate independently. Doing this efficiently requires automation, which scales best with a marketplace of B2B services to get all sorts of work done.

There are enormous staffing shortages in health care that drive outrageous costs for human beings to do tasks essential to our care. However, increasingly, many of these tasks actually can be done at scale by others just as an Uber ride to the HLTH convention involves APIs for payment (Stripe/Braintree), navigation (Google Maps), and communication (Twilio).
Similarly, every healthcare provider will be able to access via APIs for high-quality and scaled services in areas like scheduling, pre-authorization, patient payments, clinical decision support, remote care management, Rx delivery, and referrals to a plethora of other care providers, who themselves are able to take part in a seamless care journey because everyone can access and contribute to the same datasets. Devoted CEO Ed Park, commenting on a draft of this post, noted that what makes The Two As important is that they can accomplish specific tasks right when they are needed, such as a doctor confirming that a pre-procedure checklist has been completed or a patient finding out precisely where to go for a lab result [2].
Embrace The Failure of Imagination
As Chris Dixon has shown, new innovations usually run into the obstacle of humans’ inability to really comprehend all that technology can do once it has been invented. When the telephone was invented, people at first said, essentially, “Wow, that’s cool, but no one will use it because the telegraph already handles everything.” When the TV was first built, no one could think of anything to do with it initially other than film plays with one camera. No one thought about multiple cameras or going outdoors, let alone adding special effects. It was a failure of imagination, which tends to accompany any new breakthrough technology.
Healthcare now faces the same failure of imagination. Why shouldn’t the care plan sit not just on your smartphone but also on your watch to remind you when it’s time to take medication, to tell you when your activity levels do not align with your exercise goals, and to reach out proactively with a loving AI-driven voice to ask you how you’re doing and give you the opportunity to share your experience, gain reassurance, and make sure you are moving in the right direction with your behaviors, which are as vital to your health as anything? I don’t know what will come of a world where data and care can be unbundled and fully synchronized, but I’m quite sure it will involve profoundly beneficial innovations.
Modern healthcare organizations will innovate based on access to complete data. They will depend vitally on rapidly emerging foundation models and AI tools to support care delivery. Furthermore, a proliferation of services can be integrated into their platforms by technologists using a simple line of code that references these multifaceted services.
The Four Ds and The Two As will bring us a health care future that is unrecognizable today. Crucially powered by privacy and consent, each patient will be able to choose a medical home that is always-on and available, which can help navigate a marketplace of specialized providers/services/apps based on individual care plans.
All-in-One Care To Integrate Digital and Terrestrial Delivery
The goal is a seamless, all-in-one care experience that is delivered via a broad marketplace of providers who can offer tailored care to our individual needs; just ask Lionel Richie.
Many people have comorbidities, which require thoughtful guidance and planning from knowledgeable care providers, which is the heart of primary care. But these care providers do not need to operate inside the bowels of large medical buildings that are hard to find without access to complete information about your care, including the care that has been provided to you outside of their own four walls.
There will be a plethora of data sources that will complement these decisions, including “omics” and diagnostic data and even data from wearables and patient reported outcomes. Today, this data often frustrates care providers because they lack the training to utilize it effectively and do not have the time to incorporate it into your care planning. Hence, they will depend on AI to do the long slog of reviewing data tirelessly, understanding implications for the care plan, looking for deviations of key measures from safe thresholds, and then making the work easy for the care provider to integrate into the care plan and provide the patient with the right advice and new recommendations to keep us all on the right track .
If the goal is to Live to 100, or Die Trying, this will be achieved only with a modern digital care architecture that is convenient and low cost. This system must harness the full power of AI to continuously monitor your health while you enjoy life, only interrupting you when necessary to keep you on the right track. Health equity demands that healthcare is made radically more accessible, effective, and affordable. A world where data has a prominent role, treated as essential to your care as a doctor, lab, or pharmacist, is a crucial first step. However, only with automation powered by AI and API-related services can anyone keep up with the demands of healthcare and deliver the quality of care you deserve.
So, let’s build a new health system where anything a provider or a patient needs is accessible via automation, powered by the data that is crucial to each person’s health. With the right infrastructure at our disposal, all it will take is some imagination.
Bluebird Kids Health
Bluebird Kids Health reimagines pediatric primary care in underserved communities. They’re on a mission to provide exceptional care, so that every child can thrive. Their innovative pediatric value-based care model provides comprehensive, evidence-based care, tailored to the unique needs of each family. They strive for exceptional health outcomes, reduced medical costs, and an unparalleled experience for children, families, and their dedicated care teams.
F-Prime’s Summer Internship and Fellowship Program: Meet Our 2024 Interns and Fellows
A big thank you to our interns and fellows for their valuable contributions this summer!
This summer, F-Prime was excited to welcome a talented group of interns and fellows to our Cambridge office. They played key roles in competitive landscape analysis, sourcing, founder calls, and more. Read on to discover what it’s like to be part of our internship and fellowship programs.
“I loved the constant drive F-Prime had for solving healthcare’s toughest problems. I also appreciated the mission-driven aspect of the investment process, focusing on clinical outcomes as well as the ROI a company could provide. As someone who has now worked on the VC and hospital side of the table, I am excited to see VC firms like F-Prime pushing the innovation envelope in healthcare and working with hospitals, government, payors, and others to make the healthcare system better for everyone.”
“This internship solidified my aspiration to work within venture capital, because of the dynamic nature of the industry, the intellectual challenge of assessing companies and management teams and the innovative approaches founders are taking to solve complex challenges. I’m looking forward to applying my Masters education to invest in and support entrepreneurs in the tech sector.”
“I primarily worked on a landscaping project where I compiled bispecific assets in development for inflammation and immunology, and identified several promising lead assets for potential investment opportunities. Additionally, I contributed to the scientific due diligence of ongoing deals, led several interviews with key opinion leaders (KOL), and participated in introductory calls with prospective biotech companies. I truly enjoyed the process of identifying the “gold” among the vast assets in development through scientific due diligence and KOL interviews. It was incredibly rewarding to see how my efforts in scientific due diligence contributed to an investment decision.”
“I wanted to explore a career option in the biotech industry for after I finish my PhD. I did a landscaping of Th2 immunity in the central nervous system, attended many intro calls, helped diligence companies of interest, and presented to the team on certain companies or spaces of interest.”
“I learned about F-Prime summer fellowship opportunities through LinkedIn and joined F-Prime as a summer fellow due to my interest in exploring alternative career paths after graduation, as well as my enthusiasm for gene editing and drug delivery. F-Prime has a remarkable portfolio of companies focused on addressing clinical unmet needs with these technologies. I also joined to gain insight into VC’s perspective on the future of next-generation therapies.”
“I mainly worked on the commercial assessment for a new portfolio company. As part of this, I built an epidemiology model of the disease area, assessed potential market dynamics and exit opportunities, and created a revenue forecast. I most enjoyed working with the new portfolio company team – each person had unique expertise that they were happy to share, and I learned so much from them throughout the course of the project.”
“I learned about F-Prime through a family friend. I decided to join as an intern because F-Prime gets to work with amazing biotech startups and help them grow as a business. Additionally, the culture at F-Prime is extremely friendly and everyone at the firm wants to help you be the best version of yourself.”
Applications for our 2025 program are not open yet, but if you are interested in learning more, please send an email to careers@fprimecapital.com.
Behind the Build: Q&A with Tammy Sun, Carrot Fertility
Tammy Sun, the Founder and CEO of Carrot Fertility, is a pioneering leader driving transformative change in global fertility care. With a profound commitment to comprehensive and inclusive services, Carrot Fertility addresses the diverse needs of individuals navigating their family-building journeys and beyond.
Navigating the complex landscape of women’s health and fertility care demands an inclusive and personalized approach—a principle that aligns closely with Carrot’s mission. Tammy highlights the diverse needs of those facing fertility challenges, emphasizing the critical role of tailored support amidst a sea of information, costs, and legal considerations. Carrot’s innovative model encompasses the full spectrum of fertility and hormonal healthcare, pioneering a lifecycle approach that transcends traditional boundaries.
As Carrot continues to expand its offerings and educate members, Tammy remains steadfast in her pursuit of transforming reproductive health and family-building care on a global scale.
What motivated you to start Carrot Fertility?
In my 30s, I decided to freeze my eggs. I was surprised to learn that despite having a great job and health insurance, my three rounds of egg freezing wouldn’t be covered. I spent more than $35,000 out-of-pocket.
While the overall experience was emotionally challenging, I also felt grateful that I had enough money in savings to pay for my care. That’s not true for most people who undergo fertility treatments. Cost is one of the biggest barriers to accessing care, and I was set on changing that. Carrot’s mission was born from this vision of fertility care for all, inclusive of age, sex, sexual orientation, gender identity, race, income, marital status, and geography. Today, we are the leading global platform for comprehensive support and access to care for maternity through menopause — and pre-pregnancy through parenting.
Can you tell us a bit about the women’s health landscape overall? What makes fertility care so complex? Why is an inclusive, personalized, and comprehensive approach necessary for those experiencing infertility?
While fertility and family-building care is a fundamental part of healthcare, there’s no one-size-fits-all approach. Some people know they want to grow their family but aren’t sure where to start. Others have begun the process but have encountered challenges and need guidance on what step to take next. The experience is unique for everyone, but with so much information out there – and other added complexities, including navigating costs and local laws and regulations – it can be challenging for an individual to understand what’s best for them and their personal needs. That’s why we work directly with our members to create personalized Carrot Plans that guide members every step of the way.
How does Carrot stand out from other women’s health players? What current gaps is the company fulfilling?
What sets Carrot apart is our global and inclusive approach. We are the first organization to demonstrate an international presence since day one. We have reached into more than 130 countries and offer end-to-end translation of the Carrot app (web, iOS, Android) in ten languages, allowing employers to offer unilateral benefits.
Carrot is also the only fertility benefits platform that focuses on the full lifecycle of fertility and hormonal healthcare – from fertility preservation, treatments, and pregnancy to menopause and low testosterone for healthy aging. We have the largest provider network to support members globally, no matter their age or journey.
How has F-Prime supported Carrot in getting to where it is today?
Carl and the F-Prime team have been instrumental in Carrot’s journey by deeply understanding the significance of enhancing health outcomes through improving access to high-quality, lifelong fertility care. Since joining Carrot’s board in August 2020, Carl has been a key strategic partner when navigating challenges and seizing opportunities in the ever-evolving healthcare landscape. Carl’s strategic approach, coupled with his profound expertise, has guided us toward success for our customers, partners, and most importantly our members.
How did you come up with the company name?
First-generation fertility products were largely cycle tracking-related and feminized in their naming and branding. We knew early on that fertility was a human healthcare issue — not only a women’s health issue. Carrot is easy to say, easy to recognize, and we’re continuing to build a brand around the name that invites all people to engage in lifelong fertility and hormonal healthcare.
What’s been the most rewarding part of your tenure with Carrot to date?
Hearing directly from our Carrot members. We support people throughout some of the most meaningful times in their lives, and we don’t take that for granted. Whether it’s hearing from members who adopted their son, a member who was able to work with a postpartum doula, or a member who could now afford to freeze her eggs, each and every one of these personal stories means so much to me, and our team. It’s the most rewarding part of our work.
What’s the best piece of professional advice you’ve ever received?
One of the best pieces of advice I ever received was from a friend, who sadly passed away a few years ago. She was a daring, brilliant, and successful entrepreneur. She was also an author who published a best-selling book not long before she passed away. I once asked her why she decided to write a book and she replied, “because I could no longer not write one.” She had something she thought she could give the world. Similarly, there was a point when I could no longer not start a company whose mission is to bring fertility care to all people. This is the advice I’d pass on to anyone thinking about embarking on a journey to build an enduring company. Do it, but only if you think there’s no other pursuit you can, or should, be doing instead.
What are your near-term and future goals for Carrot? How do you see Carrot supporting expanded access to fertility and family building care?
We continue to focus on expanding access and improving outcomes for our members through personalized care. That includes educating our members about their options and guiding them to the right level of intervention based on their needs.
With preventive options like fertility testing, ovulation tracking, and nutrition support, we encourage members to approach their fertility health proactively. Two-thirds of Carrot members choose less invasive options over IVF when appropriate, eliminating costly and medically unnecessary procedures.
For cases where IVF is the best option, Carrot members are educated on the benefits of single embryo transfer (SET), which is the single most predictive indicator of a singleton IVF pregnancy and subsequent successful live birth. It is an important clinical protocol used to avoid multiple gestation pregnancies, which are associated with higher medical costs and poorer health outcomes for mothers and infants.
Last year, we published an internal study, also validated by independent actuarial service Milliman, demonstrating the highest reported SET rate of any fertility benefits vendor and an IVF pregnancy rate greatly exceeding national averages. The study found that Carrot’s SET rate of 93% was 27% higher than the national average and that our IVF pregnancy rate of 60% is 11% percent higher than the national average. Our industry-leading SET rate leads to a reduced risk of low-birth-weight deliveries and costly NICU admissions, ultimately reducing overall healthcare costs.
What makes you most hopeful about the impact that Carrot could have for women when it comes to family building and beyond?
Over the last few years at Carrot, we’ve launched new products and expanded our offerings to ensure our members have access to care, no matter what fertility, pregnancy, hormonal health, or family-building journeys they’re on. One product I’m particularly passionate about is our menopause support.
By 2025, 1.1 billion women worldwide will have experienced menopause. Symptoms can last for years and disrupt daily life, yet menopause is rarely discussed at work despite it impacting women at the height of their careers. In fact, 80% of women cite menopause as a workplace challenge and more than half have considered making an employment change due to menopause.
We were the first fertility benefits platform to introduce menopause support, and now, nearly all of our 1,000+ customers have started offering the benefit to their employees, showing promise that the tides are turning towards more menopause support in the workplace. I’m hopeful that a year from now, we’ll see even more leading employers recognize the need for menopause support and that it becomes a standard part of healthcare benefits.
Jessica Chen, M.D.
Jessica Chen, M.D., is a Venture Partner at F-Prime and the Chief Health and Wellness officer of ThriveWell™, an umbrella company committed to promoting health, wellness, and longevity nationwide. Her mission to enhance people’s well span incorporates a holistic, community-based approach to care that moves beyond a typical clinical setting and focuses on purpose, healthy eating, exercise, spirituality, and preventive medicine. She also incorporates her personal experiences into her work. ThriveWell’s MRS Diet, for example, was inspired by Dr. Chen’s approach to feeding her own family. M, mostly plant-based. R, real whole foods. S, stop eating before you are full.
Dr. Chen perfected her holistic approach to care as the Chief Clinical Officer at ChenMed, a nationally recognized full-risk healthcare organization serving more than 200,000 patients across 15 states. At ChenMed, Dr. Chen helped implement a care model that reduced hospitalization by 30 to 50 percent and helped patients live, on average, five to seven years longer than their non-ChenMed counterparts. She then led the company’s clinical, recruitment, onboarding, training, and leadership programs; inspiring new generations of physicians to achieve the same results through a doctor/patient relationship built on trust and influence. Her efforts to achieve a culture of high-quality outcomes were instrumental in ChenMed being named to Fortune Magazine’s 2020 Change the World list, the only healthcare delivery organization so recognized.
Dr. Jessica Chen holds a doctorate degree from the University of Miami and completed her residency in Internal Medicine at UM/Jackson Memorial Hospital. She is actively involved in Nicaragua Medical Missions, a Christian non-profit organization that provides medical assistance to underserved communities in Nicaragua. She is married to her medical school sweetheart, Dr. Gordon Chen, ThriveWell’s Chief Executive Officer. Together, they have four children.
Gordon Chen, M.D.
Gordon Chen, M.D., is a Venture Partner with F-Prime and the Chief Executive Officer of ThriveWell™, an umbrella company committed to promoting health, wellness, and longevity. The organization employs integrated, holistic offerings through two unique brands that provide concierge-style outcome-based medical care with access to an exclusive facility for motivated adults to maximize their healthspan (BLU By ThriveWell), and a proactive approach to home care that keeps members active, eating right, mentally engaged, and productive (ThriveWell At Home).
Dr. Chen discovered how adults benefit from outcome-based, longevity medicine within a community-based environment that focused on purpose, nutrition, movement, and spirituality when he and his family built out ChenMed, America’s leading primary care provider for older adults. As the organization’s Chief Medical Officer, he helped over 200,000 older adults across 15 states significantly improve their outcomes and gain 5-7 healthier years.
Dr. Chen is also an accomplished author, co-writing “The Calling: A Memoir of Family, Faith and the Future of Healthcare,” which outlines his family’s story and their vision for proactive, transformative care. A graduate of Brown University and the University of Miami Miller School of Medicine, as well as a preventative cardiology expert, Dr. Chen is deeply involved in charitable work, supporting medical missions in Nicaragua and at-risk youth through his family’s non-profit, Youth Impact Center. He is married to his medical school sweetheart, Dr. Jessica Chen, ThriveWell’s Chief Health and Wellness Officer and former Chief Clinical Officer of ChenMed. Together, they have four children.
Xaira Therapeutics
Xaira Therapeutics is an integrated biotechnology company driving advances in artificial intelligence to learn the language of life and transform how we treat disease. The company seeks to rethink the drug discovery and development process from end-to-end by bringing together leading talent across three core areas: machine learning research to better understand biology, expansive data generation to power new models, and robust therapeutic product development to treat disease.